|
|
Can stem cell treatments for arthritis bring relief to those suffering from the disease? For all of human time, the swelling and aching of joints has been a common experience. As connective tissue breaks down over time, the result is stiffening, pain, and immobility. The three most common causes of arthritis include joint injuries, age-related wear and tear, and autoimmune disorders. While some people are luckier than others, few people seem to escape it entirely, which is why stem cell treatments for arthritis are intriguing to so many.
Today, the most common kinds of arthritis are osteoarthritis (OA), rheumatoid arthritis (RA), and psoriatic arthritis (PA).
Because BioInformant is a publisher of stem cell industry news, we understandably don’t offer stem cell treatments. However, our Founder is a stem cell patient, and as a company of analysts, we do our best to track this evolving industry. With this context, let’s dive into how stem cells are currently being utilized for the treatment of arthritis in novel and intriguing ways.
In this article:
- Is Stem Cell Therapy for Arthritis Still Experimental?
- What Is Arthritis?
- Why Is Arthritis Traditionally Hard to Treat?
- How Can Stem Cells Help?
- Where Do Stem Cells Come From?
- How Do Physicians Harvest Stem Cells?
- What’s the Difference Between Autologous and Allogeneic Stem Cell Transplants?
- Can We Actually Cure Arthritis?
Understanding Stem Cell Treatments for Arthritis
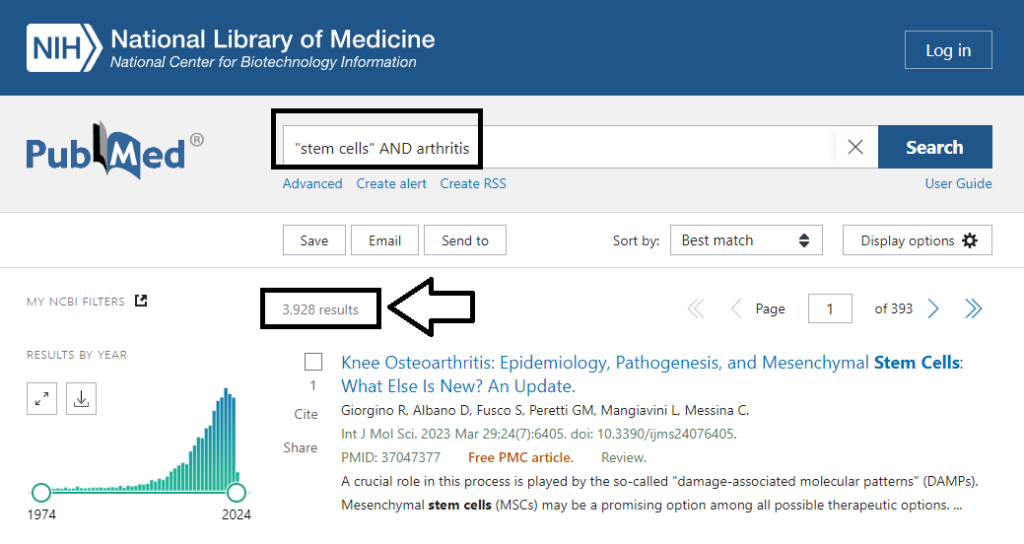
First, it’s important to know that the science around stem cells for arthritis is evolving in real-time. To date, there have been an astounding 3,900 paper published about the use of stem cells for the treatment of arthritis. The screenshot below, taken on March 5th, 2024, is from PubMed.gov, the world’s largest repository of references and abstracts on life sciences and biomedical topics. The U.S. National Library of Medicine maintains this incredible database.
It confirms that peer-reviewed papers about stem cells and arthritis have proliferate in recent years, spiking to an all-time high in 2021 and then reducing slightly in 2022 and 2023, most likely due to pandemic-related shutdowns.
Importantly, there have also been an incredible 510 clinical trials that have explored this topic, which you can see in the screenshot below taken from ClinicalTrials.gov on March 5th, 2024.
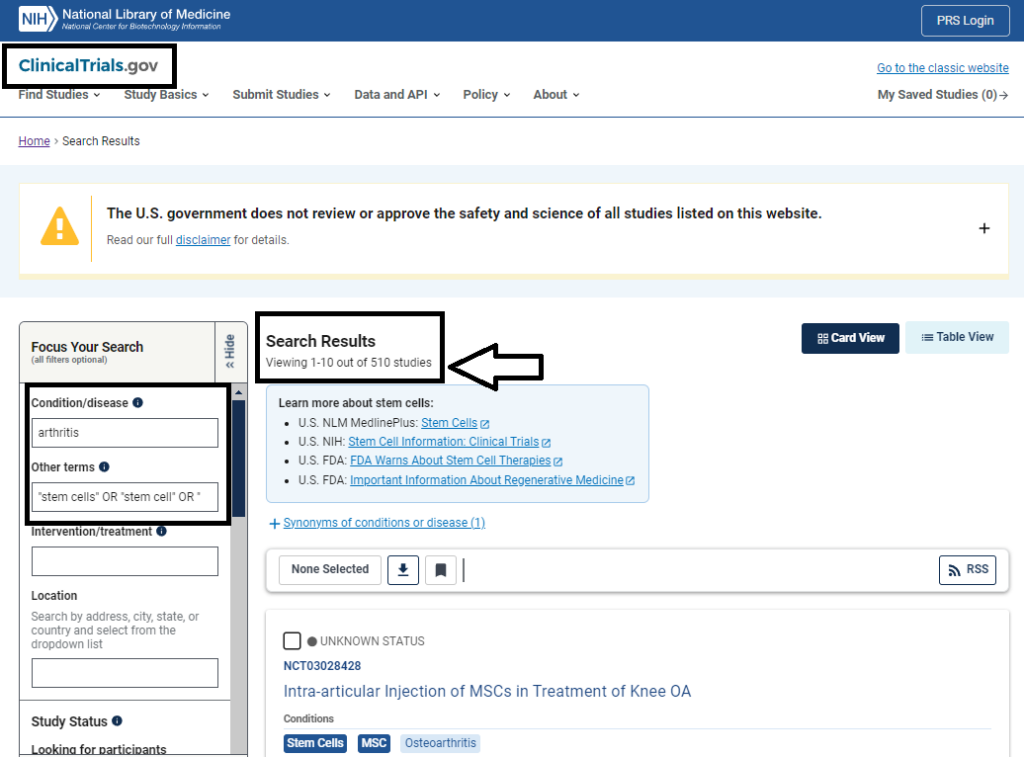
The relevance of these findings is that the scientific community and the medical community are very interested in this area of study.
Now that you know the current status of the scientific research and the clinical trials underway worldwide, let’s explore what this might mean for you.
Are Stem Cell Treatments for Arthritis Experimental?
Researchers have come a long way since the experimental days of stem cells two decades ago. New clinical trials show promising results in using stem cell therapy to treat rheumatoid arthritis, osteoarthritis, and other variants.
Those who have arthritis, or who are concerned for loved ones who do, should first understand the details of what arthritis is. It’s also good to know how stem cell therapy works and how effective treatments are. With that information in hand, readers will have enough knowledge to make an informed decision about their own treatment options.
What Is Arthritis?
According to the Arthritis Foundation, more than 50 million adults and 300,000 children have a type of arthritis, the onset becoming more likely with age.
Arthritis is not a single disease, but rather a broad category that includes a huge range of conditions. The stereotypical image of arthritis is the bent and knobby hand, but arthritis can affect any joint. What the perception and reality of arthritis have in common is severe pain and swelling of the joints, as well as relative resistance to treatment.
The condition results as frequent inflammation causes cartilage and other protective joint tissue to break down over time. Without tissue there to cushion bones, they rub against one another, causing pain and limited mobility.
Why Is Arthritis Traditionally Hard to Treat?

Because of the loss of tissue that the body can’t replace easily (or at all), no cure for arthritis has existed. Cartilage is a tissue for which replacement has been limited. While the body will try to repair damage as well as it can, it’s not very skilled at making new joint tissue.
This explains why even young and healthy people who have sustained a serious injury to a limb or hand often experience pain and limited function in the joints long after the rest of the structure has healed.
Cartilage is not like other tissue, explains the National Institute of Biomedical Imaging and Bioengineering. It does not have its own blood supply, which means it cannot readily bathe the area, nor deliver healing agents such as oxygen, growth factors, and other nutrients to the area. Cartilage that gets damaged, therefore, tends to stay damaged.
Up to this point, physicians have had limited resources to draw from when it comes to treating arthritis and other inflammatory diseases. They can recommend home therapies, such as heat and cold and ointments, but are often forced to advise patients to resort to rudimentary treatments, including anti-inflammatory drugs or other stronger medicines. If the patient does not respond to those, surgery may be an option. However, since cartilage never truly heals, the benefits of surgery are also limited.
Truly, it has long seemed as though no therapy can resolve arthritis.
Until now.
How Can Stem Cells Help with Arthritis?
With regenerative medicine comes the possibility to treat conditions once thought of as an unavoidable result of aging.
Why? Because stem cells enable the body to make new tissue, including types that it normally does not manufacture in an adult human. Cartilage is one such type, though other examples include neurons, heart cells, and more.
Stem cell treatment for arthritis could change all that. Stem cells are undifferentiated cells, present in large quantities in fetuses and newborns, but diminish with age. Those undifferentiated cells are capable of turning into a wide array of differentiated, specialized cells, given the right instructions and environment.
The real wonder of stem cells is not just that they can replace lost tissue—it’s that some stem cells types have the ability to keep dividing over time, unlike normal cartilage cells. This means not only can they fix the current condition, but they can continue to manage the arthritic area for the rest of the person’s life.
Other stem cell types, such as a type known as a mesenchymal stem cell (MSC), are highly effective at exerting therapeutics effects in the area at which they are administered. The effects of these stem cells include reduction of inflammation, reduction of scarring (fibrosis), and healthy management of the immune response.
In other words, with proper stem cell therapy, physicians can help the patient produce new cells to “fix” the injured area permanently or allow stem cells to reduce pain by limiting inflammation and regulating a healthy immune response. From a hand to a foot to a knee to an elbow, there is an answer.
Where Do Stem Cells Come From?
In order to use stem cells to heal arthritis, of course, researchers and physicians first have to extract those cells from the body.
While almost everyone knows that stem cells exist in large numbers in human embryos, many people are opposed to using embryos in medicine (even if they’re manufactured in a lab and harvested at only 3-5 days old). For those who prefer a different route than embryonic stem cells, good news: There are several other options. These include:
- Cord blood, which can be collected from newborn babies at the time of birth – Cord blood is rich in a type of stem cell known as a hematopoietic stem cell (HSC)
- Stem cell banks, where concerned citizens have donated their tissue for use by others – Many parents donate cord blood to public stem cell banks after their babies are born
- The body itself, which is a rich source of adult stem cells – Stem cells are present in a wide range of adult tissues
For those who desire stem cell treatments, their own body is the first and best place to look. The human body is packed with adult stem cells, which live in bone marrow, blood, fat tissue, the liver, the teeth, the skin, intestines, and other places.
Those found in blood and bone marrow are known as mesenchymal stem cells, for instance. These are capable of transforming into a wide array of cells and tissues, particularly those of the musculoskeletal system. They’re also helpful for patients who have blood-borne diseases or leukemia, for instance. Physicians can also use these stem cells for patients suffering from arthritis.
There exist two other main areas from which to harvest adult stem cells, explains Arthritis-Health, and that is blood and fat tissue. Researchers have dubbed those that come from fat tissue, adipose-derived stem cells (ADSCs).
Once they have the stem cells fully prepared, the physician will give the patient an injection. The cells begin to double and populate within area, creating a therapeutic response. Which raises the question, how do physicians harvest stem cells and manufacture the stem cell injections?
How Do Physicians Harvest Stem Cells?
In order to provide stem cell treatment for arthritis, physicians must first retrieve stem cells from the body. Typically, physicians remove stem cells with a needle from fat tissue or blood. In the case of bone marrow, the patient may receive a local anesthetic or get lightly sedated. That’s because inserting a needle into bone is very painful.
In the “cell replacement approach” to treating arthritis, a physician must then coach the cells toward becoming the right kind of stem cell.
Remember, in their undifferentiated state they are capable of becoming any number of different cell types. To turn them into cartilage cells, scientists in the lab must send them signals to differentiate. Once the stem cells have differentiated, researchers cultivate them until they have enough, then inject them back into the patient.
Alternatively, the physician may use a “signaling approach” to treating arthritis.
In this approach, stem cells such as mesenchymal stem cells (MSCs) are retrieved from one site within a patient’s body where they are found in plentiful supply, such as within the fat (adipose) tissue or bone marrow. After isolating the cells within a laboratory, they are re-administered to the patient through injections into the site needing repair.
In the days after these stem cells are administered, they exert positive therapeutics effects on their local environment. For arthritis patients, this is often a joint, where the stem cells act to reduce inflammation, swelling, and pain.
What’s the Difference Between Autologous and Allogeneic Stem Cell Treatments?
Again, there exist multiple options in terms of whom to get stem cells from: a manufactured embryo, another adult, cord blood, or oneself. The two main categories, however, are the patient’s own body and someone else’s. These are called, respectively, autologous and allogeneic transplants. Both are effective in some cases, and dangerous in others.
In the case of allogeneic transplants, when the patient receives cells from a donor, they run the risk of the donor cells attacking the body in what’s known as graft-versus-host disease. This can cause serious illness and even death, which is why the patient’s own stem cells are always preferable. Plus, there exists a guaranteed match, which is rarely the case with other people.
The main risk with using one’s own stem cells is if the patient carries cancer in their blood or other tissue. Then, they run the risk of re-transmitting it to themselves following radiation or chemotherapy, which is counterproductive. With arthritis, however, this is far less often a concern than with cancer treatments.
The Cost of Stem Cell Treatments for Arthritis
Understandably, the cost of stem cell treatments for arthritis can vary substantially depending on the patient, procedure, and location of the treatment.
However, in most cases, stem cell treatments for arthritis range from $900 to around $6,500 per treatment. When it comes to the cost of stem cells for arthritis, a major variable will be whether your arthritis is limited in scope or affects your whole body, as is the case with conditions like psoriatic arthritis.
For more information on the cost of stem cell therapies, explore this article.
Can We Actually Cure Arthritis?
It’s too early to say we can “cure” arthritis. However, several grants and research studies are now underway, and the scientific community has strong hope that this form of regenerative medicine will soon become the norm. In the meantime, those hoping to enroll in a clinical trial should speak to their doctors about suitability and next steps.
Seeking a Stem Cell Treatment?
As the world’s largest publisher of stem cell industry news, BioInformant understandably cannot provide clinical treatments or advice. For this reason, please contact GIOSTAR with your medical questions. GIOSTAR is a global stem cell company that has treated a large number of patients, both in the U.S. and worldwide.
You can reach them at this link to schedule a consultation or ask them your questions.

















Fantastic work for humanity.