Until the first FDA approval of cancer immunotherapy in 1990, the foundations of cancer treatment were surgery, chemotherapy, radiation therapy, and bone marrow transplantation. For more than a decade, immunotherapy has gained worldwide acceptance as the “fifth pillar” of cancer treatment.
Immunotherapy enlists and strengthens the power of a patient’s immune system to attack and kill the cancer cells. Within the human body, T cells are a type of white blood cell that support immunity. There are 25 million to 1 billion different types of T cells within the human body. These cells fight against anything foreign that enters the human body.
Oncologists typically avoid using phrases such as “game changing” or “groundbreaking” when referring to cancer treatments. However, oncologists have surprisingly referred to CAR-T cell therapies as “groundbreaking immunotherapies” because this novel approach offers hope to some cancer patients where there was none before.
Even though CAR-T therapies have only been approved for a limited range of cancer indications to date, the development of CAR-T treatments for other cancers will occur over time. Over the next 5-10 years, two to three dozen different types of CAR-T therapies are likely to get approved for the treatment of various types of liquid cancers, and eventually, solid tumors.
CAR-T Cell Therapy Development
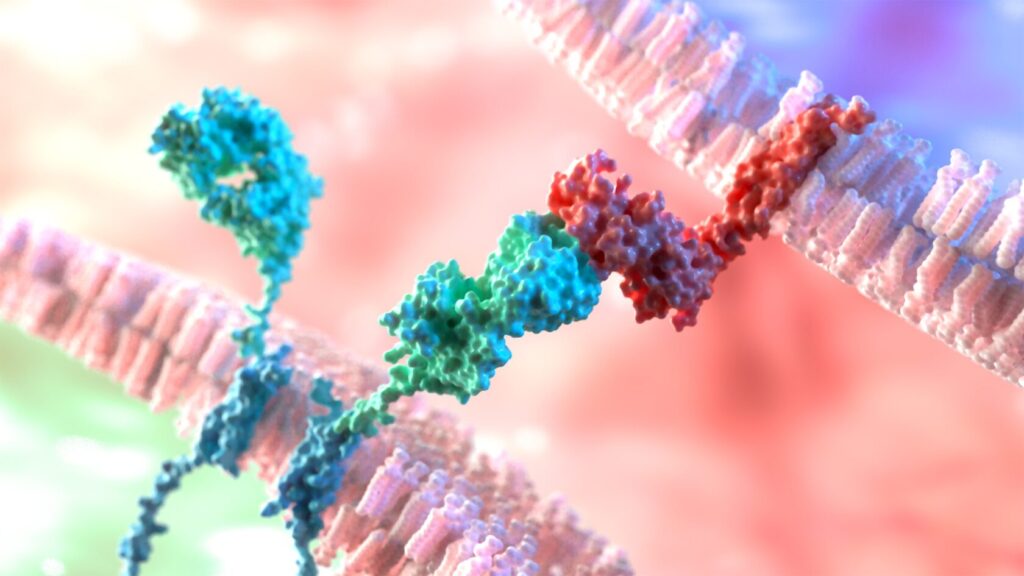
CAR-T cell therapy involves the collection of lymphocytes or T cells from cancer patients and genetically modifying them within the laboratory. The modified T cells, called CAR-T cells, are armed with a new receptor that makes the T cells able to seek and destroy the cancer cells. Because CAR-T cells are “living drugs”, a single infusion can destroy large numbers of tumor cells. CAR-T cells can also multiply themselves in vivo (within the body) and move from one cancer cell to another until they kill the last tumor cell. Thus, CAR-T cell therapies can produce complete remission in many patients.
Indeed, from 60% to 70% of the patients treated in the earliest clinical trials are now in remission for over ten years, which is an unprecedented clinical accomplishment.
Developments within the field of CAR-T cell therapy are only the tip of the iceberg. CAR-T therapy development today feels similar to the launch of the first chemotherapy treatments fifty years ago, when oncologists had access to only a small handful of chemotherapy protocols. Today, cancer patients are being treated with more than a hundred different chemotherapy agents.
In a similar way, we are likely to have several CAR-T therapies available in the near future to treat liquid cancers, solid tumors, autoimmune diseases, and inflammatory conditions.
Although CAR-T cell therapies are highly promising, they still have hurdles to overcome if they are to reach their full potential. The most significant hurdle is a cost in excess of $350,000 per dose. For this reason, efforts are now focused on to development of a place-of-care manufacturing process as a means to cut costs. In order to eliminate the need to cryopreserve and transport cells, the industry needs to make progress in this area.
As examples of recent progress in this area, the benchtop CliniMACS Prodigy instrument from Miltenyi Biotec can produce autologous CAR-T cells just in eight days. Similarly, in March 2022, a research team in the Perelman School of Medicine at the University of Pennsylvania developed a process to generate functional CAR-T cells in 24 hours.
Strategies for the Future of CAR-T Therapies
The first round of CAR-T products were developed to target liquid cancers (leukemia lymphoma, multiple myeloma). In these cancers, the infused CAR-T cells come in direct contact with cancer cells that circulate in the blood and lymphatic system. Over time, some CAR-T cell therapy developers have shifted their focus toward solid tumors that are located outside of the circulatory and lymphatic systems.
For example, brain tumors have historically been a challenging type of tumor to treat because most cancer drugs are prevented from reaching them by the blood-brain barrier (BBB). Thankfully, recent discoveries have identified that the brain has lymphatic vessels. This means CAR-T cells have the potential to penetrate the BBB and access brain tissue, positioning them as an intriguing treatment approach for several types of solid brain tumors.
Areas of active investigation in CAR-T space include developing strategies to maximize outcomes of CAR T-cell therapies, minimize toxicities, broaden targets beyond CD19, and target solid tumors. New combination therapies are actively being considered by many researchers. It is a challenge to select better preclinical models to identify potential combination therapies.
In solid tumors, researchers are particularly interested in identifying better targets and overcoming obstacles in the tumor microenvironment which have the potential to block T cell function.
Additionally, more precise genome editing technologies, such as CRISPR, are increasingly being used to develop clinical CAR-T product candidates. Allogeneic CAR-T products are yet to reach the market, but hundreds of clinical trials, mostly in China are focusing on allogeneic products. Clinical trials are anticipated to have a broader impact as CAR-T cell therapies expands into other indications, including other cancers and frontline therapies.
What areas of CAR-T cell therapy progress appear the most promising to you? Share your thoughts in comments below.